In April 2020, a study of The Mount Sinai Hospital in New York City was conducted to better understand the challenge of adapting idealized infection control design guides to site-specific conditions during a pandemic. The study aimed to capture quick interventions that are working, offer a new hypothesis and framework to guide future design interventions, and share lessons to assist other medical facilities as they pursue their own necessary spatial adaptations moving forward. Three units repurposed for COVID-19 were studied. Using action cameras and cloud-based videoconferencing, clinicians helped designers remotely peer in real time to active COVID-19 units, create “heatmap” annotations of perceived risk by frontline clinicians, and conduct interviews with decision makers.
The COVID-19 pandemic has challenged health care systems around the world to provide safe and effective care. Leveraging spatial design, architecture, and design hacks offers an untapped opportunity to support infection prevention and improved team dynamics, ultimately improving the safety and the effectiveness of the health care team by creating an environment that supports infection prevention and team function.
Keywords: pandemic, infection prevention, spatial literacy
THE CHALLENGE
The novel coronavirus (COVID-19) has posed an unprecedented challenge to healthcare infrastructure around the world. What Dr. Paul Farmer calls “staff, stuff, space, and systems” have been pushed to their limit. There have been many stories about the crisis of stuff, staff, and systems, but fewer discussions about space. One reality that links them together is that healthcare workers—who are particularly vulnerable to exposure and more severe infection —must remain healthy in order to protect patients, families, and communities. And the design of hospital spaces must help protect us.
The space of the hospital itself however, will continue to facilitate nosocomial (hospital borne) infection, unless infection control protocols are established and adhered to (Liu 2020). And herein lies the problem: validated protocols designed to prevent COVID-19 transmission do not yet exist, and therefore hospitals are implementing spatial redesigns on the fly, doing their best to learn from protocols based on other diseases, like Ebola and tuberculosis.
Until we can better understand the virus’ pathways, we won’t be able to confidently redesign our existing spaces to adhere to new and higher standards of infection control guidelines. In the meantime, hospitals will continue to repurpose and convert their spaces adhoc to meet surge demand—adapting idealized infection control protocols to unideal spaces and situations. This means healthcare workers and administrators must quickly adapt inflexible spaces, recognizing that the resulting adaptations may put healthcare workers and our communities at risk unless we can quickly create site-specific guidelines that are adherable and implementable based on the best available knowledge. While we need research to understand who is at increased risk for complications of COVID-19 and to develop effective vaccines and best therapies, we also need research that identifies how spatial design and awareness can mitigate risk.
LEARNING FROM A FRONTLINE HOSPITAL
The following case is an example of how clinicians at The Mount Sinai Hospital in New York City, researchers, and designers came together to understand the constraints of adapting guidelines to imperfect spaces, and the lessons we believe other institutions can learn from this. Shortly after the Shelter-in-Place order was issued by the Governor of New York in mid-March, Mount Sinai transformed its entire care delivery system and carried out significant infrastructure modifications to address the COVID-19 outbreak.

Figure 1: Mount Sinai Kravis Children’s Hospital 4th Floor South Wing on April 6, 2020, photograph copyright Michael Dolinger.
This case study presents a three-week spatial research methodology that took place within a frontline hospital at the epicenter of the COVID pandemic in New York City, with the goals of:
- bringing light to the challenge of adapting idealized design guides to site-specific conditions,
- capturing quick interventions that are working,
- offering a new hypothesis and framework to guide future design interventions, and
- sharing our lessons to assist other medical facilities as they pursue their own necessary spatial adaptations moving forward.
METHODOLOGY
During the week of April 6, 2020, a team of clinicians and designers from the Mount Sinai Kravis Children’s Hospital and The Mount Sinai Hospital, MASS Design Group, and Ariadne Labs investigated spaces converted and repurposed for the care of critically ill COVID-19 patients. Drawing from MASS’s infection control design experience and evidence-based research experience, Ariadne Lab’s public health innovation pathway and knowledge sharing model, and Mount Sinai’s position on the frontlines of the NYC epidemic, the team sought to illuminate COVID-19 capacity planning, interventions, and opportunities.
Figure 2: Screenshots from virtual walkthrough of active COVID-19 patient care unit, images copyright MASS Design Group.
The rapid response spatial study focused on three units converted and repurposed for COVID-19, including adult intensive care units (ICU), an adult medical-surgical unit, and a pediatric unit. Using action cameras (GoPro) and cloud-based videoconferencing (Zoom), Mount Sinai clinicians helped designers remotely peer into active COVID-19 units, create “heatmap” annotations of perceived risk by frontline clinicians, and conduct interviews with Clinical Operations and Facilities leadership.

Figure 3: The team documented observations through on-the-fly sketches, drawing exercises, and photographs; and also generated graphics like the diagram to the far right to better depict conditions and recommendations, images copyright MASS Design Group.
Together, the practitioners, designers, and researchers identified and documented interventions, discussed our understanding of limitations, and recommended next steps to furthering a shared understanding of design interventions and strategies.
PRE-COVID-19 DESIGN STANDARDS
Many design recommendations from before the current coronavirus pandemic exist regarding idealized conditions for treating patients and protecting healthcare workers.
For highly contagious infectious diseases, negative pressure isolation rooms are the standard of care. These are single patient rooms designed with antechambers and specialized airflow precautions. To prevent contaminated air from spreading into the rest of the hospital, rooms must be fully sealed, achieve a specific number of air changes per hour, ensure negative pressure (preventing room air from entering the hallway), and safely exhaust contaminated air. For diseases spread through direct contact, like Ebola, other infection control precautions are layered on—such as carefully choreographed routes for patient and staff movement across the facility and special surface sanitization measures.
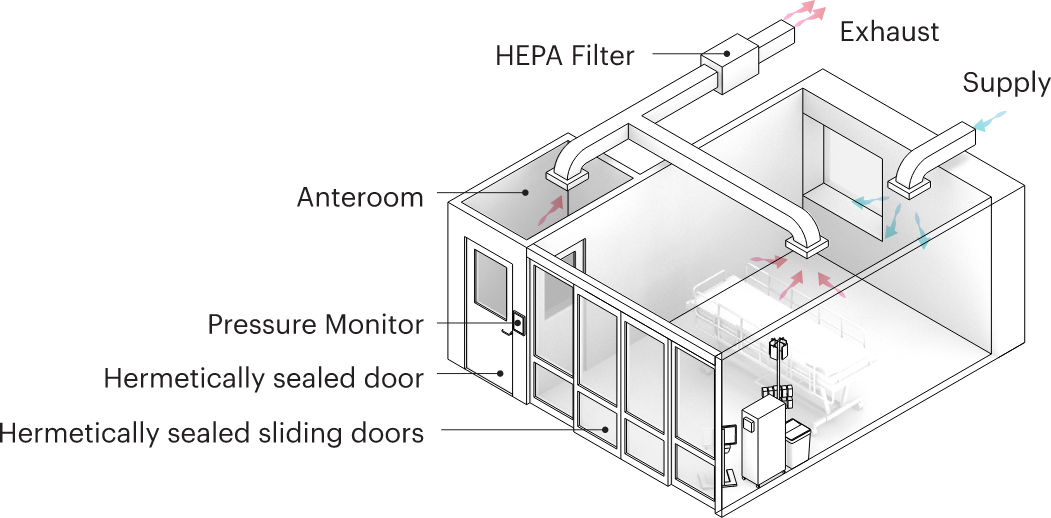
Figure 4: Diagram representing the setup of a negative pressure isolation room, image copyright MASS Design Group.
Until recently, however, hospitals have accommodated infectious disease patients as the exception, not the norm. Most large urban hospitals in America have a handful of negative pressure isolation rooms. Prior to COVID-19, and during the very early stages of the outbreak, this was enough. But what happens when a hospital needs to be able to accommodate hundreds of patients under pandemic conditions? This is what Mount Sinai faced in March.
THE MOUNT SINAI HOSPITAL
In less than three weeks, beginning in mid-March, the Mount Sinai leadership redeployed healthcare workers to COVID-19 units, backfilled the gaps by shifting provider responsibilities, implemented a new shift system to minimize risk to health workers during shift change, established complex PPE distribution and recycling systems, implemented donning/doffing practices, postponed elective procedures to create capacity for the coronavirus surge, rapidly implemented telehealth services, restructured research efforts to focus on the pandemic, and committed resources to provide ongoing support for frontline workers including childcare, transportation, and psycho-social support (Edmondson 2017).
During the same period of time, the Infection Prevention and Clinical Operations and Facilities teams at The Mount Sinai Hospital worked to significantly expand the hospital’s COVID-19 bed capacity in anticipation of a surge. The novel coronavirus forced healthcare facilities to broaden their focus from the individual patient room to the entire care unit. Mount Sinai built a 100-bed step-down care unit in the hospital’s atrium (Figure 5), and in partnership with Samaritan’s Purse erected a temporary 68-bed tent facility (Figure 6).

Figure 5: Photo showing the step-down care unit, photograph copyright Michael Dolinger.

Figure 6: Photo showing the temporary tent facility, photograph copyright Michael Dolinger.
SPATIAL MODIFICATIONS DURING THE SURGE
The hospital additionally converted 260 existing patient rooms into negative pressure isolation rooms. Within adult ICUs designated for COVID-19 care, tremendous changes took place. Walls and doors were constructed across the front of previously open ICU bays, and measures were taken to ensure fully sealed patient spaces. Large high-efficiency particulate air (HEPA) filter units were brought into rooms and set up to directly exhaust out windows that were fitted with wood panels. Intravenous fluids and patient monitors were pulled out into hallways to minimize provider exposure and allow for safer and easier monitoring (Figure 7). PPE waste and recycling bins were dedicated to each unit, and protocols were established to bring these materials to dedicated service elevators in an effort to minimize cross-contamination.
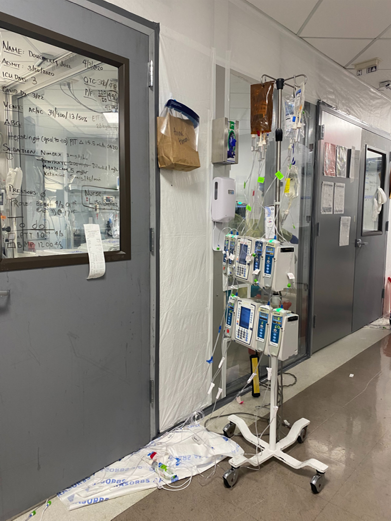
Figure 7: IV fluids and monitors in the hallways, photograph copyright Michael Dolinger.
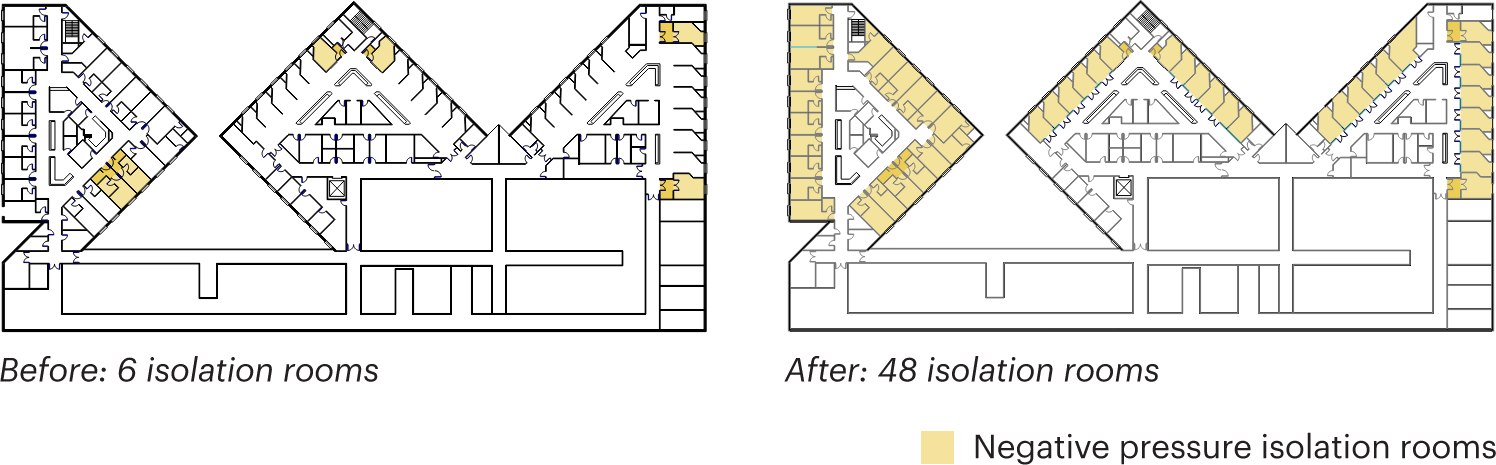
Figure 8: Negative pressure isolation rooms on 6th floor of Guggenheim Pavilion, image copyright MASS Design Group.
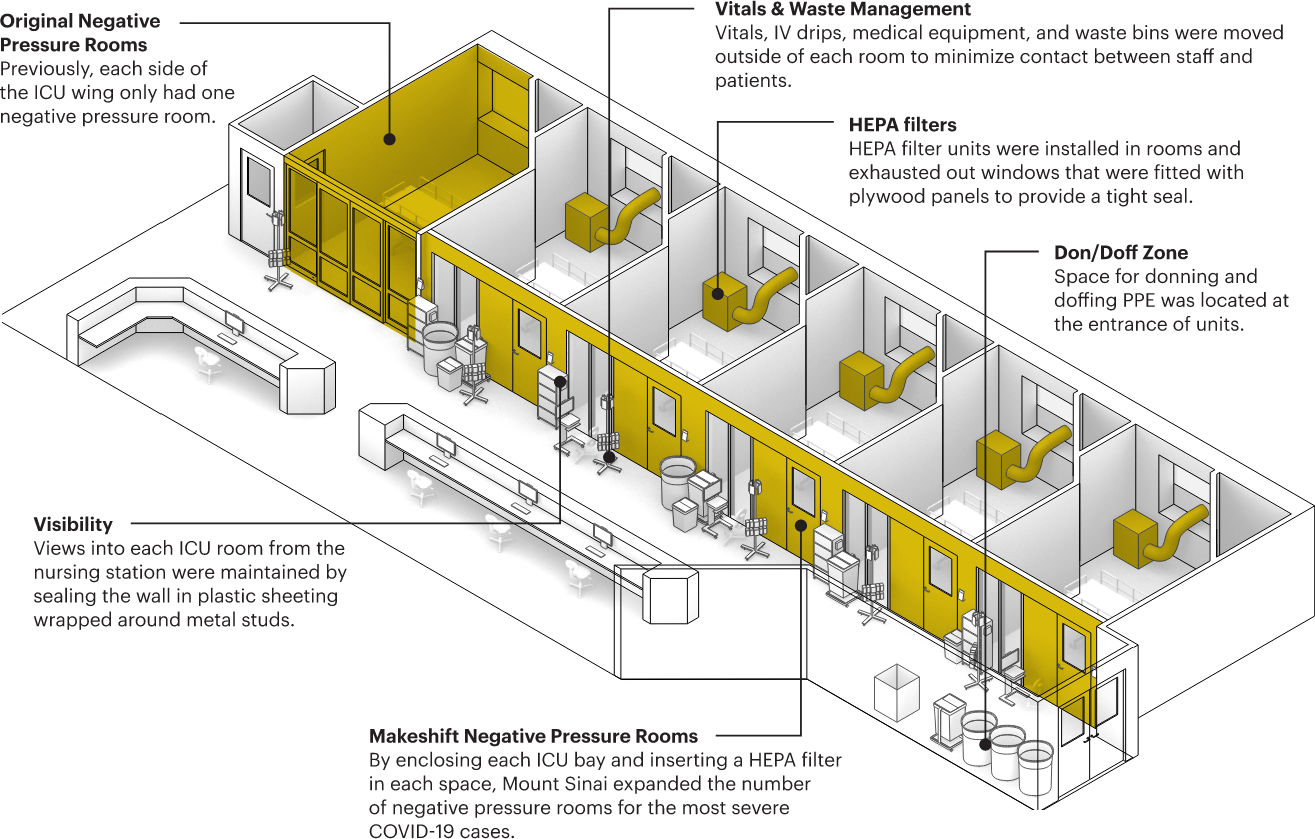
Figure 9: Diagram of interventions on the Guggenheim Pavilion highlighting different interventions that were made to turn this adult ICU wing into one that could treat patients who have tested positive for the coronavirus, image copyright MASS Design Group.
DESIGN HACKS
Mount Sinai’s administrative, Clinical Operations, and Infection Prevention teams worked together to create physical changes to reinforce the programmatic and behavioral protocols implemented on COVID-19 floors. Specifically, they sought to include visual cues at key moments of risk or transition: for example, doors into patient rooms, PPE storage and access locations, and thresholds between different areas of risk. In some places, they installed signage indicating “extended use PPE zones,” designated boxes for recycling face masks, and installed additional hand sanitizers to signal to staff upon entering or exiting key thresholds. These physical or cognitive “anchors” helped to designate functional use of space and reinforce patterns of work within these constraints. Other anchoring mechanisms could include tape on the floor, signage, and intentionally placed whiteboards or paint.
Stations to access PPE were provided at key locations, which in turn affected how and where healthcare providers utilized the equipment. PPE carts and instructional signage were located on every COVID-19 unit, a brown bag system was created to designate and store face masks for individual providers, and a peer approval system was implemented—requiring nurses to fill out a donning/doffing record sheet with “buddies” signing off on proper PPE application (Zimring 2018). Additional interventions that may increase PPE adherence in the future include: demarcating designated “clean” zones around PPE carts and donning areas, creating more predictable placements for essential equipment and resources, making access to PPE less high-touch, and developing a more consistent system for brown bag storage (either consolidated near the unit entrance, or affiliated with specific patient rooms).
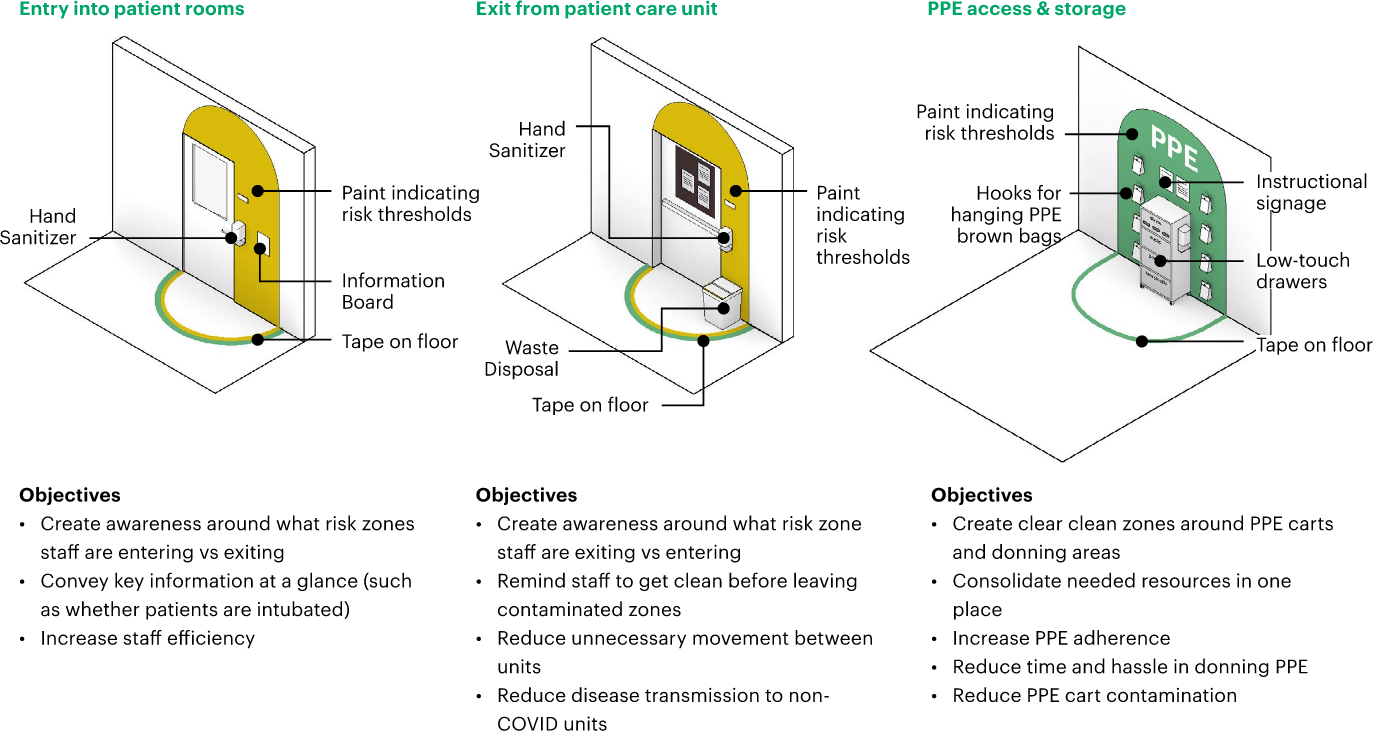
Figure 10: Design Hacks, images copyright MASS Design Group.
COMPLIANCE GAPS AND IMPLEMENTATION CHALLENGES
Even with Mount Sinai’s ingenuity and innovation in achieving a radical transformation in a short timeframe, adapting the existing hospital proved to be a difficult task. Changes were ultimately bound by inherited and inflexible infrastructure. Within adult ICU units, it was not possible to integrate antechambers due to the spatial constraints of the floorplan, as well as the need to maintain direct visibility and access to patient rooms for high-level nursing care. Shifting IVs and monitors outside the patient room was necessary, but created more congestion in the corridors. And while the HEPA filtration fixtures were necessary, they took up an immense amount of space within patient rooms and were loud, constraining staff movement, communication, and workflows.
In older, smaller buildings like those that housed the pediatric units, repurposing spaces for coronavirus care was even more challenging. The presence of larger clinical care teams (reflecting higher nurse-to-patient ratios and more ancillary staff), alongside the need to minimize staff exposure within patient rooms, meant that more providers were working in hallways and compromising spatial distancing.
In buildings laid out without centralized nursing stations, this prompted the distribution of individual nurse computer stations along the hallway. Combined with the addition of PPE carts and recycling bins, as well as more complex cleaning and disposal protocols, the result was hallways crowded with equipment (Figure 11). Particularly in critically ill patient spaces, this left little room for clinician rounding to comply with social distancing recommendations, and introduced inefficiencies that made nurses’ work slower.

Figure 11: Mount Sinai Kravis Children’s Hospital 4th Floor South Wing, photograph copyright Michael Dolinger.
Beyond the size, layout, and flexibility of units, spatial perception emerged as another important factor. Clinician discussions and floor plan annotation exercises revealed inconsistent perceptions of risk zones within units, and the need for stronger spatial cues. Unlike typical care contexts, where providers work on units they are familiar with, and with teams they are familiar with, COVID-19 providers may be working for the first time in new spaces, collaborating with new team members, and may even be providing a type of care that is not their specialty (for example neonatologists caring for adult ICU patients). In medical decision-making, providers have been trained to weigh the level of risk against the potential for positive outcomes. But within COVID-19 units, the risk level of different spaces is not always clear or something clinicians consciously think about.
DEVELOPING SPATIAL LITERACY
Terms like spatial literacy (Tversky 2019) are underutilized in the research world but are especially prescient in a moment like this. As individuals, our spatial literacy around our bodies and our proximity to others has been unexpectedly heightened over recent weeks. The simple act of asking a clinician to annotate a heatmap by color-coding spaces to infection risk was revealing. The exercise generated interesting discussion and helped clinicians deeply consider space in a new way and rethink existing assumptions. The heatmap created for the pediatric COVID-19 unit also made visible an important design challenge: controlling movement across units. Particularly in tight, vertical healthcare settings, like the Mount Sinai Kravis Children’s Hospital, healthcare teams needed to leave units in order to access key shared spaces like nurses lounges, or fetch resources like drugs or supplies. To limit nosocomial infection between COVID-19 and non-COVID-19 units, thresholds between floors (i.e., elevators and stairs) needed to be considered more closely, but proved difficult given the constraints in this building.
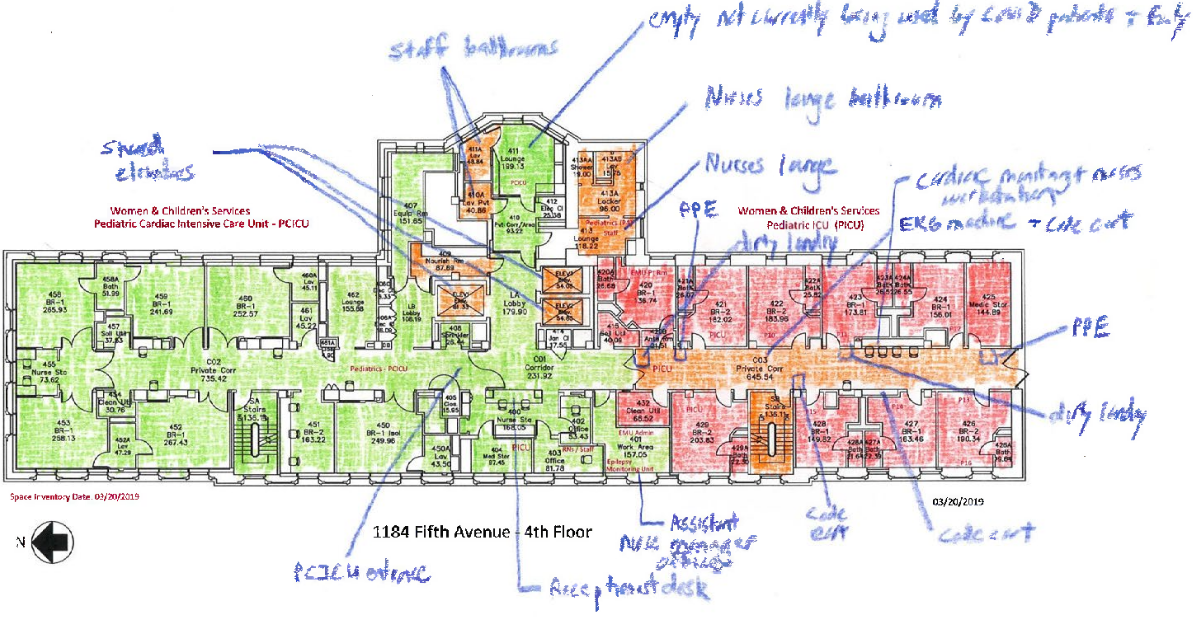
Figure 12: Annotated floorplan of pediatric COVID-19 unit by Mount Sinai clinicians.
Annotated heatmaps of the adult ICU units revealed significant differences in individual perceptions of risk zones. This is notable because staff behavior is typically most stringent in areas perceived as red zones, where the risk of contagion is perceived as high; but there were varying degrees of adherence to infection control rules in spaces perceived as orange or green, and differing levels of legibility of which spaces carried high risks of contagion.
Because of this ambiguity, “warm zones” may be dangerous for healthcare workers simply because they are not aware that they are warm zones. In warm zones, healthcare workers might overlap with staff coming from or going to other floors, or on-call clinicians might be changing personal protective equipment (PPE).
At a bare minimum, health facilities can leverage design cues to clearly mark orange areas as “warm zones” and convey expected behavior to healthcare workers within these areas. At the same time, they can implement active interventions to try and lower infection transmission in these areas—that is, turning orange spaces into green ones.
We asked three different clinicians to annotate heatmaps of ICU units on the same floor (Figure 13). Their drawings revealed three very different perspectives on risk.
- “Hot” areas known to be contaminated, where providers should use full infection control precautions and be on alert (red color in drawing).
- “Clean” areas that are fairly confidently non-infected areas, where staff can use relaxed precautions (green color in drawings).
- “Warm” or unclear areas that may actually pose risk even if not perceived as a risk zone (orange color in drawings).
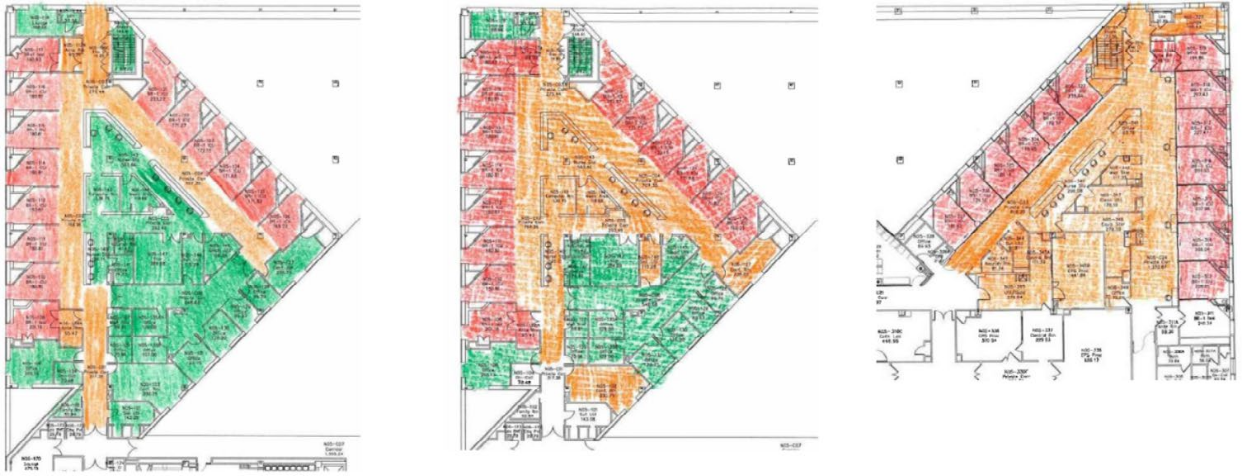
Figure 13: Heatmaps of ICU units on the same floor by Mount Sinai clinicians.
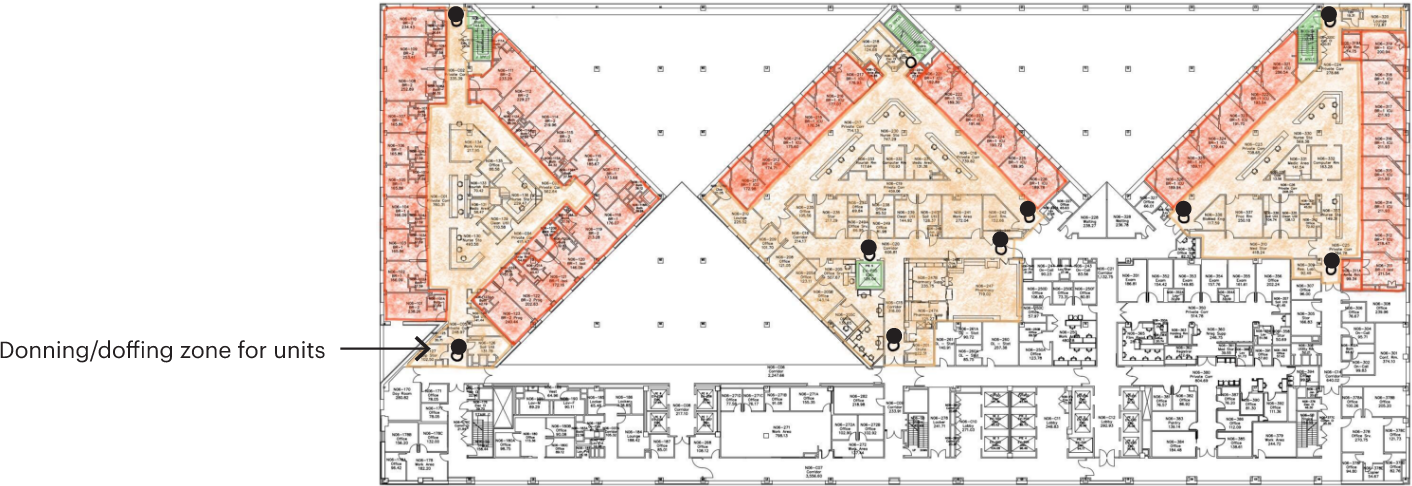
Figure 14: Risk zones of an adult ICU floor during pandemic surge conditions, sketch shows the zones in the Med-Surg and ICU units on 6th floor of Guggenheim Pavilion, image copyright MASS Design Group.
Together in conversation with staff at Mount Sinai, the research team identified red, orange, and green zones under pandemic surge conditions. In the condition of a massive increase in infection control rooms, the entire unit effectively becomes an orange zone, and clearly marked donning and doffing areas need to exist at major entrances to the unit, in addition to patient room thresholds (Figure 14). All possible measures should be taken to ensure that stairs and elevators in vertical hospitals stay uncontaminated, as they connect many different zones; and tape, signage, or paint can be used to designate these different risk areas and thresholds more clearly.
CONCLUSION
While revised infection control practices have been quickly adopted, medical facilities are not configured to adapt easily to these rigid adherence protocols. Instead, they are forced to respond “on the fly” in situ, often with insufficient amounts of equipment, protective gear, or clear guidelines. Amidst heroic efforts to transform hospital-wide clinical processes and infrastructure, adaptations can vary floor to floor and unit by unit, often revealing design “hacks” that are both creative and discordant. Nevertheless, hospitals are not designed for pandemic surge, and existing infection control protocols are inadequate for COVID-19.
KEY TAKEAWAYS
More research and strategies in partnership with healthcare staff and designers are needed to help develop spatial literacy among providers and to use the built environment to facilitate this knowledge. Thoughtful spatial interventions can help create situational awareness for COVID-19 units, set clear and consistent protocols for thresholds, align appropriate behavior within well demarcated risk zones, and identify opportunities to more safely and flexibly expand capacity during surge conditions.
- While infection control protocols are being quickly adopted, hospitals are not designed to easily pivot to support the infrastructural changes needed at the scale of a pandemic surge. One major shift is the focus from individual patient care to unit care, creating caregiving processes for COVID-19 units that place a heavy reliance on interstitial spaces. This lesson means that enforcing proper infection control protocols in hallways and key thresholds, like entries into units, may be as important as in patient rooms.
- Variability exists both in the adaptations from floor to floor and unit by unit, as well as in personal perception of risk zones within care units. These differences affect how health workers behave and interact, sometimes introducing new elements that may impact the risk of infection among staff and patients.
- Spatial literacy (i.e., the ability to read and understand space) can be a powerful tool to orient healthcare workers within unfamiliar and rapidly-changing COVID-19 caregiving environments. Simple visual aids and design nudges can help mitigate infection transmission by clearly conveying risk zones, creating mental “anchors” for specific activities, and aligning behavior with policy. Design can help advance the sociology of infection control, along with our developing understanding of its biology.
These interventions are needed now, but they will not be short-lived. And they will be even more necessary in hospitals with fewer resources. Thoughtful and simple spatial adaptations can help create situational awareness for COVID-19 units, set clear and consistent protocols for thresholds, align appropriate behavior within well-demarcated risk zones, and identify opportunities to more safely and flexibly expand capacity during surge conditions.
As we continue to realign care infrastructure and processes to the new normal, clinicians, designers, and administrators must work together to make invisible risks more visible, and create spaces that instill order, collaboration, and morale.
MICHAEL DOLINGER, MD, MBA is currently the chief fellow of pediatrics at Kravis Children’s Hospital at the Icahn School of Medicine at Mount Sinai where he is also a fellow in the department of Pediatric Gastroenterology and Hepatology. He has previously performed successful research on physician and trainee wellness and burnout, and social network analysis among healthcare teams.
ASHLEY MARSH, RA, is a licensed Architect currently with MASS Design Group, where she’s advancing COVID research in health, culture, and education settings for organizations across the US and generally leads strategic development along with consultative pre-development and readiness projects. She has deep experience conducting research in the built environment and designing user experience strategies for large, complex organizations, including previously leading research for San Francisco International Airport’s Revenue Enhancement and Customer Hospitality (R.E.A.C.H.) initiative. She has been named ‘40 under 40’ by the San Francisco Business Times, an Emerging Leader from the Design Futures Council, previously presented her research at forums like EDRA and SCUP, has held teaching positions at the Hasso Plattner Institute of Design at Stanford University and the Boston Architectural College, and was awarded the $10 million XQ Super School Prize for her research work on the future of the American public high school in Oakland, CA.
NOTES
Acknowledgements — Thank you to the following authors, contributors, and thought leaders who have lent their insight and support to this research project: John Bucuvalas, MD, Vice Chair of Faculty Affairs and Professor of Pediatrics, Icahn School of Medicine at Mount Sinai and Mount Sinai Kravis Children’s Hospital; Regina Y. Chen, Sr Director, MASS Design Group; Grace Galvin, MPH, Assistant Director, Innovation Platform, Ariadne Labs; Jeffrey Mansfield, Director, MASS Design Group; Michael Murphy, Co-Founding Principal and Executive Director, MASS Design Group; Neel Shah, MD, MPP, Assistant Professor of Obstetrics, Gynecology and Reproductive Biology at Harvard Medical School, and Director of the Delivery Decisions Initiative at Ariadne Labs; David Reich, MD, Professor of Anesthesiology, President and Chief Operating Officer of The Mount Sinai Hospital; Maimuna Sayyeda, Director of Operations for Mount Sinai Kravis Children’s Hospital; Amie Shao, Principal, MASS Design Group; Steven Yung, MD, Medical Director of Quality and Safety for Mount Sinai Kravis Children’s Hospital
REFERENCES CITED
Edmondson, Amy C., and Jean-François Harvey. Extreme Teaming: Lessons in Complex, Cross-Sector Leadership. Emerald Group Publishing, 2017.
Liu, Y., Ning, Z., Chen, Y. et al. “Aerodynamic analysis of SARS-CoV-2 in two Wuhan hospitals.” Nature 582, (2020) 557–560. https://doi.org/10.1038/s41586-020-2271-3
Tversky, Barbara. Mind in Motion: How Action Shapes Thought. Basic Books, 2019.
Zimring CM, Matić Z, Wong Sala MF, et al. “Making the invisible visible: Why does design matter for safe doffing of personal protection equipment?” Infection Control and Hospital Epidemiology 39, 2018: 1375-1377. https://doi.org/10.1017/ice.2018.206
